Preimplantation genetic testing is an advanced method for identifying which embryo(s) are most likely to implant and become healthy babies. The technique involves the removal of a small number of cells from each developing embryo, which are then tested to identify those having the normal number of chromosomes before transfer into the uterus. A similar process can be used for couples who are at high risk for conceiving a child with a genetic disease, to identify the embryos that are unaffected and suitable for transfer.
The Genetic Testing Process
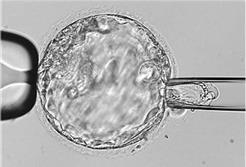
Preimplantation genetic testing is performed on cells removed from each of the embryos that reaches the blastocyst stage (day 5-6 after fertilization). To obtain the cells, a small opening is made with a laser in the membrane that surrounds each embryo (called the zona pellucida), over the region of the embryo that will become the placenta (called the trophectoderm), leaving the region that will later become a fetus undisturbed.The opening allows some of the cells to protrude where they can be separated from the remainder of the embryo.
The embryos are then frozen until the results of genetic testing are known, followed later by a frozen embryo transfer of an embryo then known to be chromosomally or genetically normal.
Preimplantation genetic testing increases the likelihood for achieving a pregnancy and also decreases the risk for a miscarriage, because the most common cause for failed implantation or miscarriage is a chromosomal abnormality. When performed to identify specific genetic disorders, it helps to avoid the need to terminate a pregnancy or the birth of a baby with a serious genetic disease.
Genetic testing performed to identify embryos with the correct number of chromosomes is called preimplantation genetic screening (PGS), and testing that is performed to identify embryos that carry a specific disease-causing gene mutation is called preimplantation genetic diagnosis (PGD).
Improvements in Technique
Over recent years, the techniques involved in preimplantation genetic testing have improved greatly. There is now substantial medical evidence to demonstrate that embryo biopsy at the blastocyst stage does not adversely affect the embryo’s ability to implant in the uterus. In past years, when embryo biopsy was typically performed at the cleavage stage of development (day 3 after fertilization) by removal of just a single cell, the procedure was more traumatic for the embryo and had a negative impact on implantation. It also was less accurate because the testing technology at the time could only evaluate some and not all of the chromosomes. Today, later biopsy at the blastocyst stage provides a greater number of cells and also allows the embryologist to remove cells only from the region that will later become the placenta. In addition, modern genetic testing methods now allow evaluation of all 24 chromosomes (22 numbered pairs and the X and Y chromosomes). Current methods of preimplantation genetic testing are highly accurate and pose little risk to the embryo.
Indications for Preimplantation Genetic Testing
As women age, a growing proportion of their remaining eggs have chromosomal abnormalities, leading to both decreasing fertility and an increasing risk for miscarriage. For that reason, although PGS can be performed at any age, it is more often recommended for consideration for women in their later reproductive years (over age 35).
PGD is an attractive strategy for couples who are at risk for conceiving a child with a specific genetic disease. Most genetic diseases are recessive, meaning it takes two abnormal genes to cause the disease. People who have one normal and one abnormal gene are normal; they have no signs or symptoms of the disease, but are carriers of the disease. If their partner also is a carrier, together they will have a one in four risk for conceiving a child with two abnormal genes who will have the disease. With some other genetic diseases that require only one abnormal gene to cause disease (e.g., muscular dystrophy, hemophilia), one half of the couple’s embryos will be abnormal. PGD allows couples at risk to avoid conceiving an affected child.
PGD is also a good strategy for couples at risk for recurrent miscarriage because one or the other partner has a chromosomal rearrangement in which two chromosomes exchange pieces (called a translocation). Although the affected partner is normal because they have all of the necessary genetic material – it’s just in a different location – they are normal, but a large proportion of the eggs or sperm they make will have too much or too little of one of the two involved chromosomes, resulting in a chromosomally abnormal conception when that combined with the egg or sperm of their partner. PGD allows embryos that are chromosomally normal or balanced like the affected parent to be distinguished from those that are unbalanced and abnormal. Transfer of only normal or balanced embryos can greatly decrease the risk for the couple having another miscarriage.
Elective Single Embryo Transfer
Because preimplantation genetic testing identifies the embryo(s) most likely to implant and become a successful pregnancy, the procedure increases the chance for pregnancy and, importantly, also allows fewer embryos to be transferred so as to minimize the risk for conceiving a multiple pregnancy and all of their associated risks for both mother and babies.







