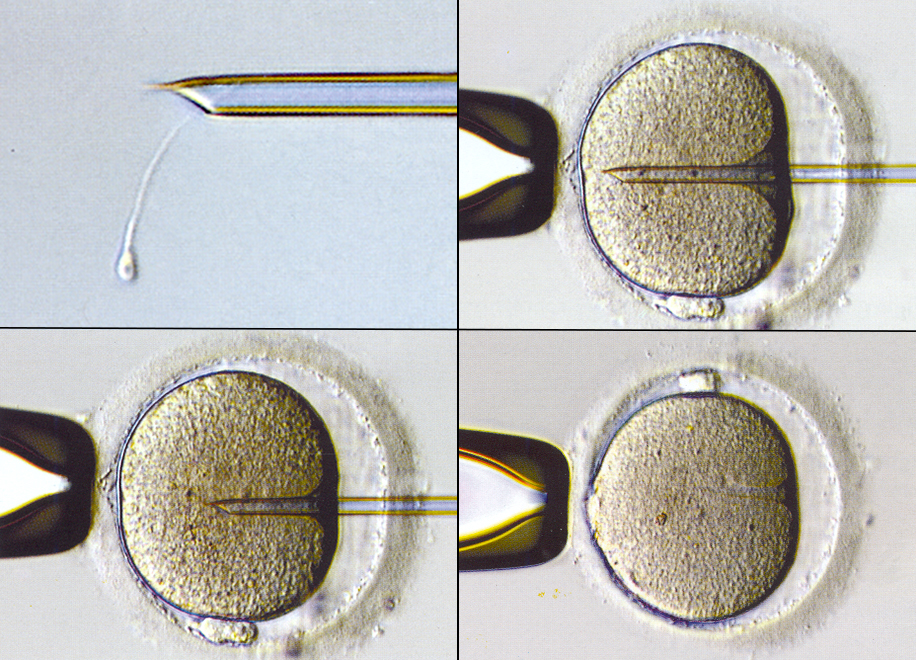
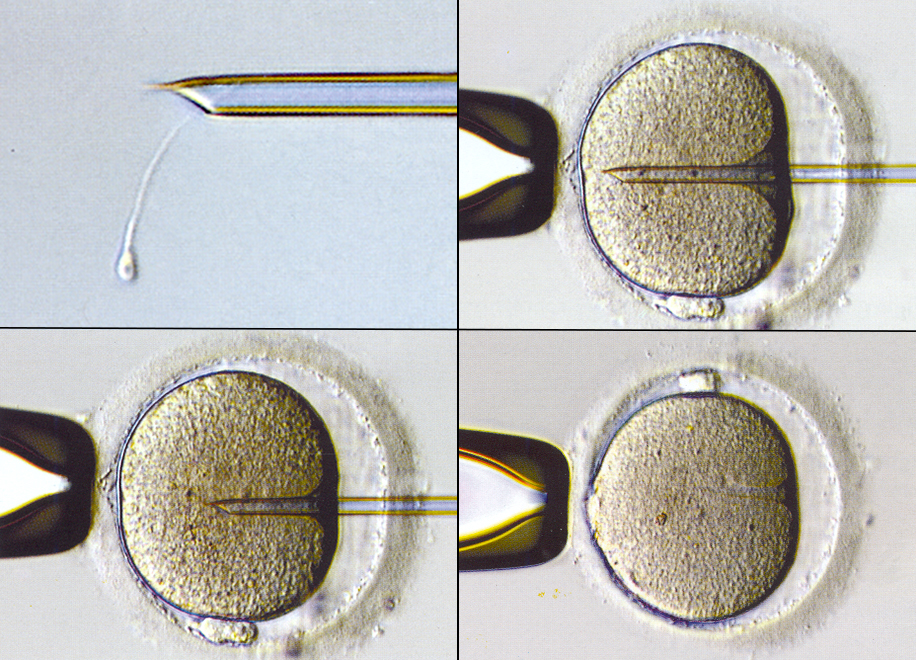
ICSI is an effective method for the treatment of male factor infertility. Instead of simply mixing sperm with eggs in the laboratory (“conventional” fertilization), ICSI involves the selection of individual sperm, which are then physically inserted into the eggs (one into each mature egg).
ICSI Process
ICSI is a specialized laboratory procedure in which individual sperm are selected from a sample, drawn up into an extremely fine needle that is inserted through the membrane surrounding the egg (called the zona pellucida), and injected directly into the egg. ICSI is used to achieve or to improve fertilization when semen quality is poor and there is reason to expect that conventional fertilization methods will yield poor results or may fail altogether. ICSI is also the method required to fertilize an egg that has been previously frozen, which can cause the membrane surrounding the eggs to harden and become more difficult for sperm to penetrate on their own.
ICSI is also the method required to fertilize eggs when using sperm that have been harvested directly from the testicles (called testicular sperm extraction, or TESE) or from the tubules surrounding the testicles (called microsurgical epididymal sperm aspiration, or MESA).
ICSI is also often recommended for couples with unexplained infertility to avoid an increased risk for poor or failed fertilization. When the number of eggs that are retrieved is relatively small, ICSI may be used to fertilize all of the eggs. When the number of eggs retrieved is greater, the eggs may be divided into two groups, with one group fertilized using conventional fertilization methods and the other group fertilized by ICSI. This approach protects against the risk of poor or failed fertilization and also provides important information about whether a sperm fertilization defect may be the cause of otherwise unexplained infertility, information that can then be used to determine whether ICSI is necessary in any later IVF cycle that may be required.
IVF with ICSI
An IVF cycle that includes ICSI involves all of the same elements as a standard IVF cycle, except that the eggs collected from the ovaries are fertilized using the ICSI method (injecting a sperm into each mature egg) instead of the conventional fertilization method (mixing of sperm and eggs together).
Success Rates
The success rate for IVF cycles including ICSI is approximately the same as IVF success rates, which suggests that the procedure has little or no adverse effect on the egg. However, experience has shown that the embryos that result from ICSI may have slightly lower quality and developmental potential. Whether this reflects the impact of the ICSI procedure or the poor sperm quality that leads to ICSI is unclear. The risk for conceiving a child with a congenital abnormality after ICSI is comparable to or only slightly increased over that observed after IVF using conventional fertilization methods. Some studies have suggested there may be a small increase in the risk for chromosomal abnormalities, compared to naturally conceived pregnancies or those resulting from IVF and conventional fertilization. Many of these chromosomal anomalies result from similar abnormalities in the chromosomes in the sperm of infertile men. Consequently, prenatal genetic testing during early pregnancy is generally recommended for women who conceive after IVF with ICSI.
Genetic Abnormalities in Men with Low Sperm Counts
Approximately 10% of men who have very low sperm counts or no sperm at all in their ejaculate may have a chromosomal defect, such as an extra sex chromosome, a structural chromosomal rearrangement, or a small missing piece of the Y chromosome (Y chromosome microdeletion). In rare cases, such chromosomal defects could result in a serious abnormality in their offspring, and because all male children will inherit their father’s Y chromosome, the sons of men having a Y chromosome microdeletion are likely to have a similar problem with infertility when they become adults. Consequently, chromosomal analysis (called a karyotype) and a special test to identify Y chromosome microdeletions are recommended for men who have a sperm concentration less than 5 million sperm/mL in their ejaculate.
The vas deferens is the muscular tubule that transports sperm from the testicles to the penis at the time of ejaculation. When the vas deferens does not form and is absent, there are no sperm in the ejaculate. Congenital bilateral absence of the vas deferens (CBAVD) is a condition highly associated with mutations in the cystic fibrosis (CF) gene and men with the condition can be assumed to be carriers of a CF mutation. If the female partner also is a carrier of a CF mutation (which in women are silent), there is a high risk (25%) for the couple conceiving a child with CF. Consequently, it is very important that the female partners of men with CBAVD be carefully and thoroughly tested to determine if they also carry a CF mutation. Couples who are at risk can choose to have their embryos tested for CF before any are transferred into the uterus. The technique is called preimplantation genetic diagnosis (PGD) and involves the removal of a small number of cells from each embryo for genetic testing. The embryos are frozen after they are sampled and remain in storage until the testing is completed. An unaffected embryo can then be transferred in a later frozen embryo transfer cycle.








